Pioneering Natasha Trial may allow children with food allergies to live without fear of a potentially fatal reaction
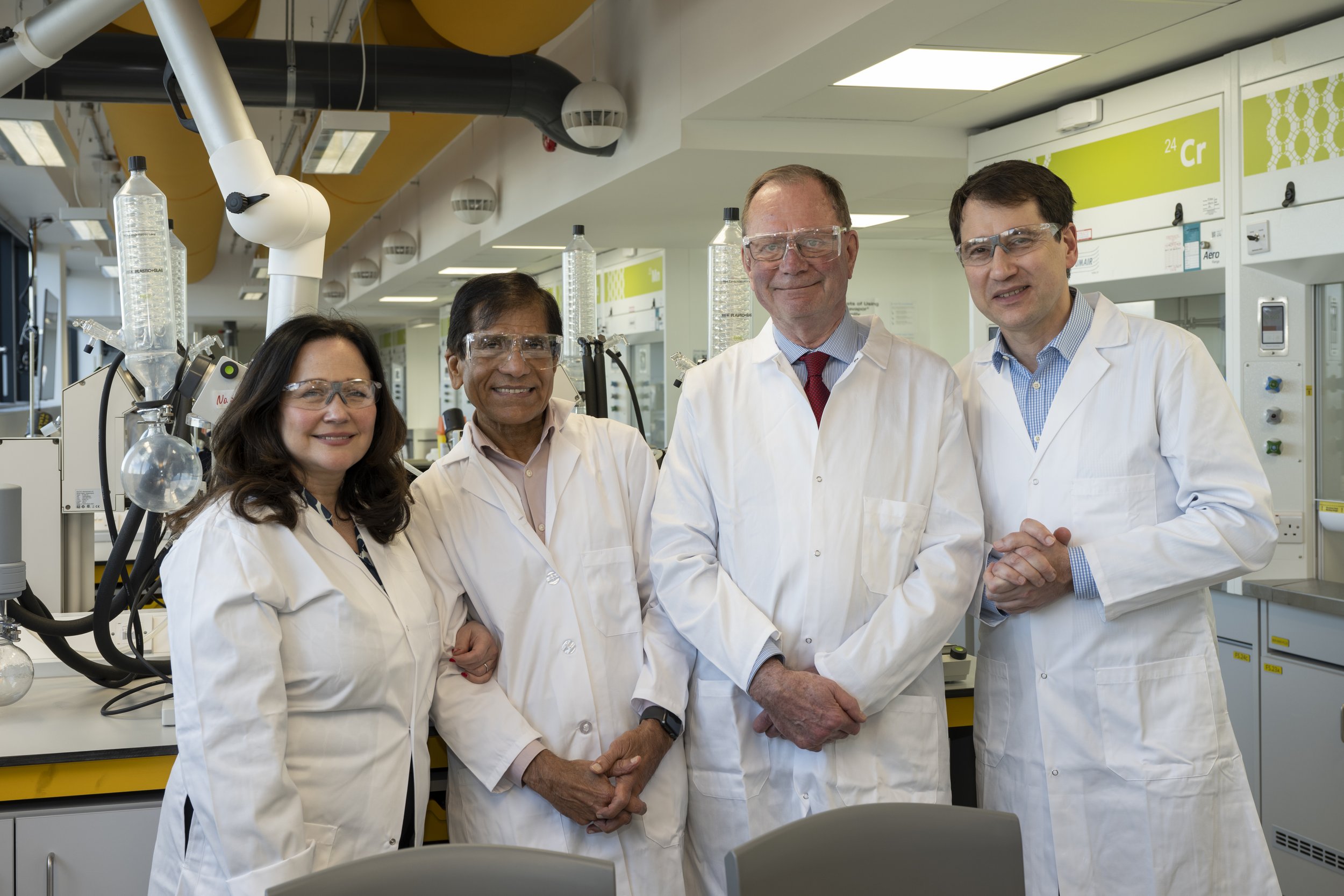
Nadim & Tanya meet the children on the Natasha Clinical Trial, in May 2024
Photo used with permission: University of Southampton
Children with food allergies as young as two are among the first participants on a new £2.7 million trial, funded by The Natasha Allergy Research Foundation, the UK’s food allergy charity
There are three groups of participants in the trial: children aged 6 to 23 with a peanut allergy, children aged 3 to 23 with a cow’s milk allergy and children aged 2 and 3 with a peanut allergy
Early evidence shows children on the trial are tolerating milk and peanuts to which they were previously severely allergic
The oral immunotherapy (OIT) trial uses everyday foods to desensitise participants to their allergies
9 NHS hospitals are taking part in the Natasha Trial. The sites are: Southampton, Leicester, Newcastle, Imperial (London), Sheffield, Edinburgh, Aberdeen, Leeds, and Bristol.
The Natasha Trial, which began in 2023, is a randomised controlled trial, the gold standard in medical research
The trial is training a network of NHS staff to offer OIT treatment
If successful, the trial will provide the evidence for the treatment to be made available on the NHS.
Results of the Natasha clinical trial are expected in 2027
If successful, this will empower the NHS to provide cost-effective treatments for people living with food allergies through oral immunotherapy.
Can you join the study?
The Natasha Trial is now fully recruited for both peanut and cow’s milk allergy – none of the NHS centres are recruiting any more patients onto the Trial.
For those of you still interested in participating in the trial, we realise this information will be disappointing. However, full recruitment means that the Natasha Trial is one step closer to completion, and once we have the results, our hope is that the NHS will make OIT available as a treatment so that people with food allergies can benefit from it.
Thank you for your support and interest in the Natasha Trial.
Photo used with permission: University of Southampton
The Natasha Clinical Trial is the first major study to be funded by Natasha’s Foundation, set up by the parents of Natasha Ednan-Laperouse, who died aged 15 from a severe food allergic reaction.
Doctors say they are already seeing children on the trial who can consume and tolerate the very foods that previously would have triggered a severe allergic reaction
Hasan Arshad, Professor of Allergy and Clinical Immunology at the University of Southampton and Chief Investigator of the trial, said:
‘We must wait until the trial is complete for the full picture but we are very pleased with the results we are seeing so far.’
Photo used with permission: University of Southampton
PARENTS of children with severe milk and peanut allergies have told us how their lives have been transformed by the pioneering Natasha Clinical Trial.
The £2.7 million trial, funded by The Natasha Allergy Research Foundation, uses daily doses of everyday food products, taken under strict medical supervision, rather than expensive pharmaceuticals to train the bodies of children and young people with food allergies to tolerate an allergen.
This approach – known as oral immunotherapy (OIT) – means children living with food allergies should no longer have an allergic reaction if they eat something which accidentally contains the food allergen, for example, due to cross-contamination.
Co-chief investigator Dr Paul Turner, Reader in Paediatric Allergy & Clinical Immunology at Imperial College London, said:
‘While introducing potential food allergens into a baby’s diet in a safe way can prevent food allergies from developing in the first place, this doesn’t always work and cannot help those who already have food allergies. We hope this study will show that using everyday foods under medical supervision can be a treatment for food allergy.’
Hospital admissions for severe allergic reactions (anaphylaxis) to food have more than tripled in the last 20 years in the UK
Offering the treatment more widely would be a huge step forward for people with food allergies and their families, and help to tackle the growing allergy epidemic.
Using everyday products to treat food allergies would also be a cheaper alternative to expensive pharmaceuticals such as Palforzia, saving the NHS money.
Photo used with permission: University of Southampton
About the Natasha Clinical Trial
Before joining the trial, the children and young people undergo food challenges over two hospital visits to confirm their food allergy diagnosis and make sure they are suitable to have the OIT treatment.
Once enrolled, each is given a very small amount of a food to which they are allergic at a dose that is safe for them, which is taken according to a standardised protocol under medical supervision. This may be given either in a hospital clinic or at home with medical support.
If they tolerate the food, they then take a daily ‘dose’ of this real food at home, and the amount is gradually increased by the medical team roughly every two weeks while closely being monitored for any adverse effects.
After between six and 12 months, the participants will reach their maximum dose. They are then monitored on this dose for a year, and the number of allergic reactions and their quality of life are compared with the control group - children with the same food allergies who have not had the OIT treatment.
In England, the trial is taking place at the National Institute for Health and Care Research (NIHR) Clinical Research Facilities located in NHS hospitals.
Results of the trial are expected in 2027.
How Oral Immunotherapy (OIT) Changed 9-Year-Old Jamie’s Life
Watch this video to hear how Oral Immunotherapy (OIT) changed 9-year-old Jamie's life.
Thomas Farmer, Image shared with permission
Meet Thomas, age 11
Thomas Farmer, aged 11, has a peanut allergy.
When he joined the Natasha Trial in Southampton in March 2023, he could not tolerate even half a peanut. By January 2024, he was eating 6 peanuts a day – a dose he will keep in his diet.
Thomas says: ‘I wanted to do the study so I can help people with the same allergy as me and to be a positive role model to others who may be going through the same as me.’
Thomas was diagnosed with a severe peanut allergy when he was aged one.
His mother Lauren says:
‘Having food allergies can be really difficult and isolating. As parents, who have lived with managing a peanut allergy for nearly ten years, we knew we wanted to see if there was a way to understand it better and help to manage the allergy.
‘Our journey on the Natasha study has been amazing so far. From day one we have felt that our son has been the number one priority throughout, and has had the best possible care given to him.
‘At first, it was very scary for both Thomas and us when he did the food challenge, as we weren’t sure what to expect. Thomas persevered and we are so extremely proud of what he’s achieved so far and continues to achieve through this study.
‘Knowing that Thomas can now tolerate six peanuts a day has taken away so much anxiety around food. It will also hopefully mean that he will be able to eat a wider variety of food as we won’t be so concerned about accidental exposure.
‘For Thomas to be able to achieve all this with no medicine – just off-the-shelf foods – is amazing.’
Grace Fisher, Image shared with permission
Meet Grace, age 5
Since joining the Natasha Trial in August 2023, Grace Fisher, aged 5 from Newcastle who has had a milk allergy since she was 2 years old, is now drinking in May 2024 120ml milk a day.
Her mother Emma said: ‘Grace is over six months into this journey and is doing amazing! She loves her daily hot chocolates.’
Grace’s mum Emma says:
‘After Grace was diagnosed with a food allergy we were constantly worried about keeping her safe.
‘Initially, I was really hesitant to agree for Grace to sign-up to the Natasha Trial. As a mum, it really worried me how safe she would be. However, as an academic researcher in public health, I knew the importance of research, reliance on participants willing to take part in randomised controlled trials.’
Grace says:
‘I think that I’m getting passed having an allergy. I love having my milk every day because it’s tasty.’
Founders of The Natasha Allergy Research Foundation -Nadim and Tanya Ednan-Laperouse OBE’s visiting the University of Southampton
The charity’s mission is to #MakeAllergyHistory through medical research, campaigning and education.
Natasha’s parents Nadim and Tanya Ednan-Laperouse, who have both been awarded OBEs for their services to charity and people with allergies, are delighted with how the trial is progressing.
Tanya said:
‘We are so happy that some children with peanut and milk allergies are already seeing the benefits of using everyday foods under medical supervision to treat their allergic disease.
‘If Natasha were alive today, this is exactly the type of research she would have loved to be part of.
‘This is a major first step in our mission to make food allergies history. We look forward to seeing the final results.’
Nadim added:
‘We can’t rely on big pharma and its giant profits to be a game-changer for people living with allergies.
‘That is why we are harnessing the support of the food industry, who have helped fund this trial, to prove that OIT can work with everyday foods, making it more feasible to be available on the NHS.’
Professor Arshad, Head of Asthma, Allergy and Clinical Immunology Service at the University Hospital of Southampton, added:
‘At present, people with food allergies are asked to avoid the food they react to and carry adrenalin pens in case of accidental exposure. This is not a satisfactory situation and we would like them to be able to live their lives without having to avoid the popular foods that others enjoy or being fearful of accidental food allergic reactions.
‘The Natasha Trial aims to do better for people living with food allergies. We are testing a clinically controlled procedure of gradual introduction of allergen foods until the point where these are tolerated. Our ultimate aim is a life without the risk of allergic reactions – reactions which for some, can be severe and life threatening.’
Dr Louise Michaelis, Consultant Paediatrician in Immunology and Allergy at Newcastle Hospitals, said:
‘Living with a food allergy can be challenging, particularly for young people who are unable to eat popular foods or have to miss out on social occasions with friends.
‘The majority of our patients have become more confident in managing their allergy since being on the trial, which is really positive to see for both the patient and their family.
‘The Natasha Trial is so important when it comes to helping patients with allergies live a fuller, more normal life. We hope that the trial will also help health professionals to understand the potential benefits of oral immunotherapy for people with certain allergies.
Sibel Sonmez-Ajtai, Paediatric Allergy Consultant and Principal Investigator at Sheffield Children’s said:
‘This study is enabling us to do something we would never have dreamed of doing before – giving patients the foods we know they are allergic to!
‘This treatment is not a cure for a food allergy, but what it achieves is life transforming. To have a patient who has had anaphylaxis to 4mls of milk to then tolerate 90mls within six to eight months is nothing less than a miracle.’
Q. What is food immunotherapy?
A. Immunotherapy is a medical treatment that uses the body’s own immune system to fight disease. It is increasingly being used to treat a range of health conditions including cancer. When used to treat food allergy, it involves giving the patient, under medical supervision, small but increasing amounts of the food to which they are allergic, so that the immune system ‘learns’ not to see the food as a threat and no longer triggers an allergic reaction. When the food is given by mouth, this is known as oral immunotherapy or OIT. The first successful case of OIT was reported in 1908 in the Lancet, a medical journal. However, it is only in the last 15 years that there has been a lot more interest in using OIT for food allergy. This has resulted in a number of research trials, which have shown it works in around 60-70% of children with food allergy to cow’s milk, egg or peanut. Despite this, OIT is still not widely available in the UK, even though a commercial product for peanut-OIT was approved in 2022.
Q. How could the Natasha Trial help people with food allergies?
A. Currently the main strategy for the 1–2 million people living with food allergies in the UK is avoiding their trigger food(s), and having adrenaline autoinjectors if they have a reaction. However, this is not a treatment, and trying to avoid the food to which you are allergic is difficult, especially when eating out. OIT offers the possibility of a long-term solution, even perhaps a cure. The aim of the Natasha Trial is to collect the longer-term data needed to establish OIT as a practical treatment for food allergy to allow people to live a more normal life.
Q. Which food allergies will be included in the trial?
A. The trial will look at OIT for two foods: peanut and cow’s milk.
Q. Is oral immunotherapy an expensive treatment?
A. OIT needs to be carried out under the supervision of a trained specialist. However, since the treatment uses everyday foods rather than a pharmaceutical pill, the cost of the treatment itself is very cheap. That is the beauty of the trial. We hope it will provide cheap, accessible solutions for people with food allergies.
Q. Is it a cure?
A. In some people, maybe. Around 60-70% of people respond to OIT and become desensitised. However, for the treatment to remain successful, most patients must continue to consume the food regularly or they lose the treatment effect. This can be challenging in some people, because they dislike the taste of the food they are allergic to. If they can continue to have their maintenance doses on an ongoing basis, then this might be a cure for some people.
Q. How is this trial different from other food immunotherapy trials?
A. Trials have already proven that OIT is effective for peanut, cow’s milk and egg allergies, particularly in young children. What we hope to do in the Natasha Trial is also generate the evidence that OIT is not only effective, but also cost-effective: by using everyday foods and showing that OIT can be done safely at home under medical advice, this will show that OIT can improve people’s quality of life and be cost-effective in the NHS. The Natasha Trial will also look at adolescents and young adults up to 23 years of age, which is different from other trials which often just include younger children. The trial is also helping to train doctors and nurses to safely do OIT, so that the NHS can offer this treatment in all parts of the UK.
Q. Why is this trial needed?
A. Despite previous trial results showing it is effective, OIT is not available in the NHS apart from for peanut using a commercial product called Palforzia. However, very few people have been treated with Palforzia in the NHS, due to the cost of treatment and patient visits. This is in marked contrast to other countries like Spain, where OIT is routinely offered to children with milk and egg allergies. The Natasha Trial will plug the knowledge gap by showing that everyday foods can be used for OIT in children and young adults with food allergies. It is a gold-standard medical trial known as randomised-controlled trial. That means some patients will receive the OIT treatment, and other won’t. This gives the researchers the best possible information to prove that OIT is successful compared to standard care (dietary avoidance) in terms of improving their quality of life, and should generate the data needed to make OIT more widely available in the UK.
Q. What about the peanut immunotherapy pill Palforzia?
A. In February 2022, the National Institute for Health and Care Excellence (NICE) approved the use of Palforzia for treating peanut allergy in children aged 4 to 17 years (this can be continued in people who turn 18 while on the treatment). This pharmaceutical product, which contains ground peanut powder, is used for OIT to desensitise patients. Studies have shown that around 60% of people treated with Palforzia were able to tolerate at least 1000mg peanut protein (around 3 to 4 peanuts), compared with just 2 per cent in those not taking the drug. While any new treatment for food allergies is welcome, Palforzia is very expensive – around £10,000 for the product itself, plus the costs of multiple hospital visits. Using real foods offers a cheaper and more accessible alternative, and also opens up the possibility of using this approach for food allergies other than peanut.
Q. Where are the trial sites?
A. The nine trial sites across the country are Bristol, Leeds, Edinburgh, Aberdeen, Leicester, Sheffield, Newcastle, Imperial College London, and Southampton.
Q. How long is the study?
A. The study is expected to run for three years.
Q. How will participants on the study be treated?
A. Participants are randomly allocated to receive either OIT or standard treatment (food avoidance). OIT is done using everyday foods which contain peanut or cow’s milk, and involves taking very small but increasing amounts of the food every day for 12 months, under medical supervision. All participants also have access to a 24-hour helpline. During the study, they will be monitored with blood tests and their quality-of-life assessed. After a year, if the OIT works, the participant is then allowed to normalise their diet but must continue to eat the food on a daily basis to maintain the desensitisation. The study will monitor how well they manage during this further year after treatment. Anyone randomised to the control group will be offered the chance to have OIT at the end of the trial.
Q. Is it safe?
A. All medical treatments carry risks and OIT is no exception. There is a risk that participants will have an allergic reaction to their daily doses of OIT. This is why OIT must be carried out under medical supervision. However, previous studies suggest it works for around 60–70% of people. The trial is not suitable for people with uncontrolled asthma, atopic dermatitis, severe allergic rhinitis, other severe and chronic diseases, and pregnant women.
Q. When will the results be published and what will they show?
A. The study is due to finish in 2027 and the results will be published once the findings have been analysed. The researchers will measure a range of factors including whether OIT is effective, improves the patient’s quality of life and whether the treatment is cost-effective.
Q. How will these results help the wider food allergy community?
A. We hope the results will provide the evidence needed to allow OIT to be offered in the NHS. If approved, OIT will offer a long-term, cost-effective solution – even a cure – for many people living with serious and debilitating food allergies. This will save lives, and offer life-long protection against severe allergic reactions to foods. It will empower people at risk of food-anaphylaxis to control their own lives and stay allergy safe using shop-bought foods rather than hugely expensive pharmaceutical products. It will also deliver the first win in the Natasha’s Foundation’s mission to Make Allergy History.